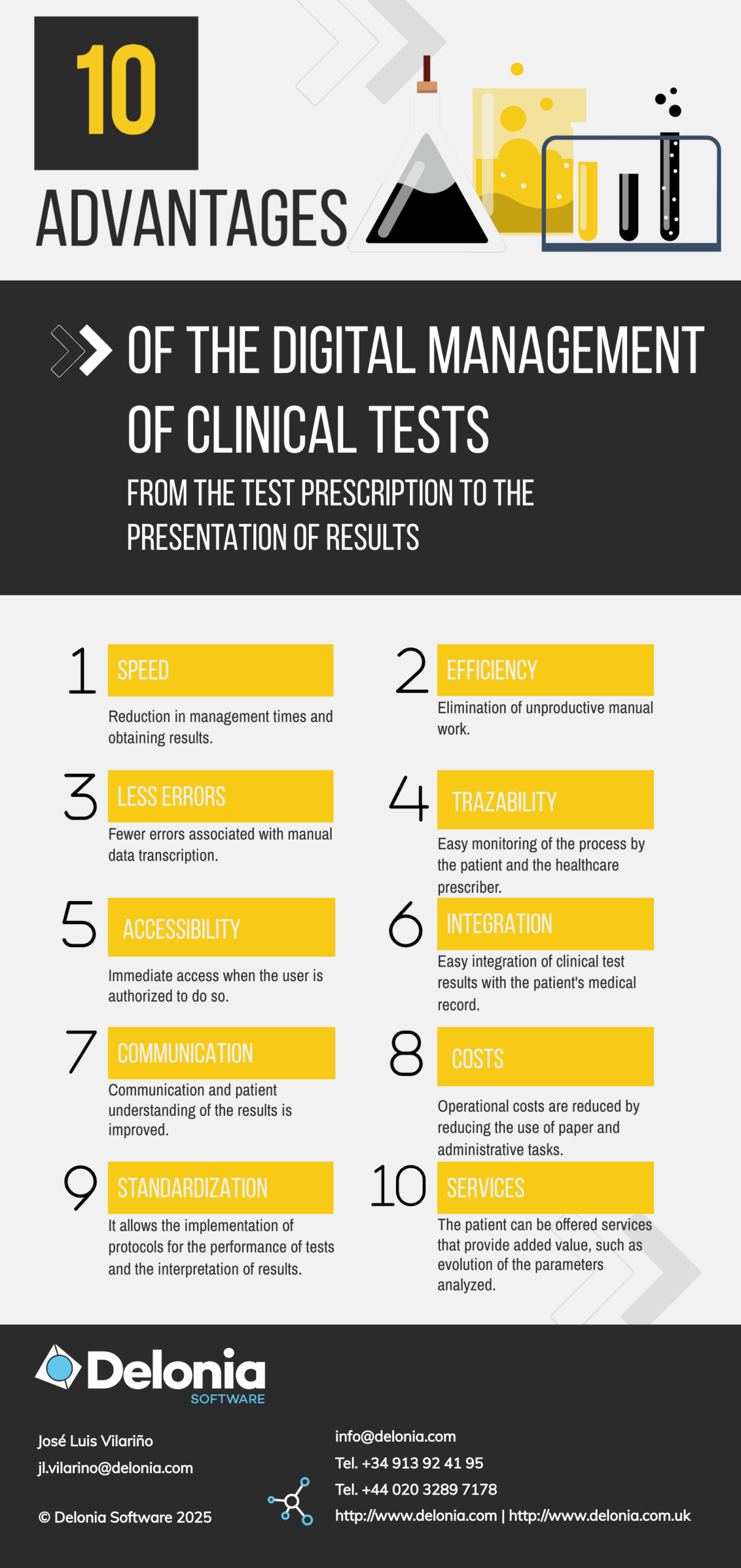
1. Why digital clinical tests
Within the digital health model that we propose, and going a little deeper into the prescription module, we are going to approach the digital management of clinical tests, a very common service in clinical practice.
In this respect, the digitalization of clinical analysis services can be seen as a priority for two reasons:
- Laboratory testing is one of the most frequently prescribed and performed services, as more than 70% of clinical decisions are based on laboratory results.
- It is a process that in practice is largely manual, which can lead to errors and failures, as well as being very costly and resource-intensive. This is especially relevant in outpatient practice.
The main idea to improve this process is to eliminate intermediate steps that do not add value between the prescribing doctor or physician and the laboratory that performs the analysis of the sample. Ideally, the necessary information should be exchanged directly between the prescriber and the laboratory, minimizing the intervention of third parties.
What information needs to be exchanged between these two parties for a clinical analysis to be performed?
- Administrative information.
- The patient’s medical conditions that justify the test.
- The determinations or parameters to be analyzed.
Among the patient’s medical information, it is always important to share the provisional diagnosis or clinical suspicion with the professionals who will perform the diagnostic tests. This will help improve clinical judgment, confirming or ruling out suspected pathologies.
2. Digital process of clinical health tests
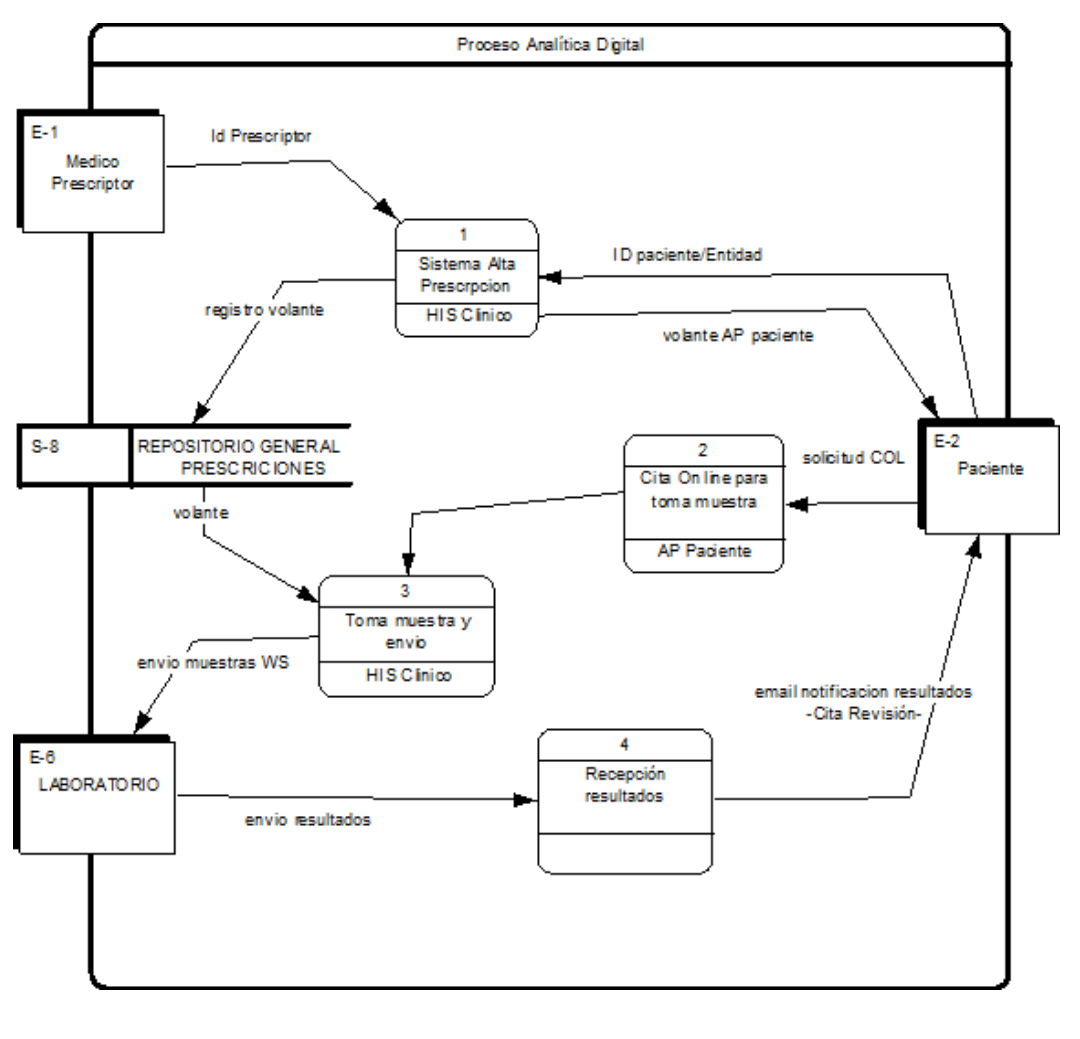
The complete digital analytics cycle, from the issuance of the prescription to the presentation and analysis of results to the patient by the healthcare professional, can be summarized in four stages:

Digital prescription:
During a patient consultation, the healthcare professional prescribes a clinical analysis from their medical record system (MRS) by selecting parameters, determinations, or analytical profiles from the system. These are stored in a specific analytical prescription data structure (commonly referred to as a laboratory test form). In our Digital MHR system, this prescription is uploaded to two environments:
- It is uploaded to the patient’s Private Area for subsequent management.
- It is stored in the general prescription repository.

Online appointment:
The patient begins the management process with the prescription, requesting an appointment for sample collection. The process would involve:
- Send an email to the patient inviting them to make an online appointment in their private area (COL).
- From the email itself, a link is proposed to the appropriate agency, suggesting available appointments soon.
- Once the appointment has been confirmed, it will be linked to the test prescription that gave rise to it.
- In this appointment, additional information can be attached to the patient with the necessary instructions and indications about the medical service to be performed.

Taking samples and sending them to the laboratory:
The patient shows up for the appointment, and the nursing department retrieves the prescription from the system and assigns the corresponding reference (barcode) to the sample tubes. This reference could be implemented in two ways:
- It could be automatically generated by the system and printed on labels.
- This reference could be pre-printed on labels (usually barcode labels) that will be read by a scanner to associate it with the prescription in the system.
Once the sample collection process is complete, the samples are sent to the laboratory through standard logistics. Furthermore, through a web service, the prescription is shared with the laboratory along with all the necessary patient information (administrative and clinical data) and the tests or profiles to be analyzed. Indeed, this management model eliminates the need to input and record laboratory test reports from the outset, meaning the task of extracting information from a paper prescription and transferring it to a digital system. This communication via web services avoids the errors that these manual processes often entail.

Collection of results:
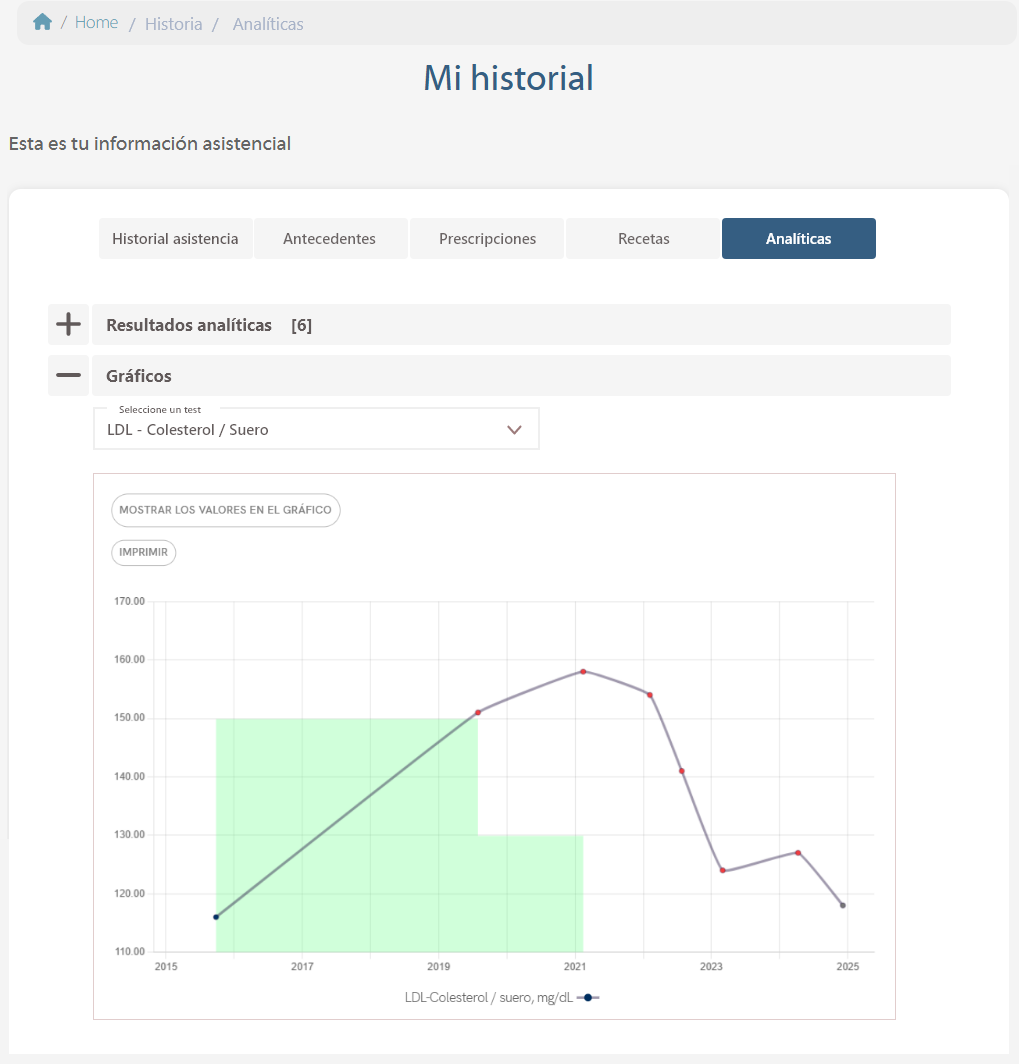
Once the samples have been analyzed by the laboratory, another web service will be enabled to publish the results and send them to the patient.
Normally, the results will be implemented by generating a PDF and an associated file with the values per determination/parameter resulting from the analysis.
When the results are published, a notification will be sent to the patient. This message will inform the patient that the results are now available by accessing their private area. This notification can also provide a link to request an appointment to review the results, suggesting that this can be done by video-consultation.
At each of the four stages, the system could be evolved using artificial intelligence (AI)-based intelligent assistants to optimize and improve both the prescription of tests and the interpretation of results.
The flowchart of the proposed process is shown below.
3. Functionalities of the clinical analysis system:
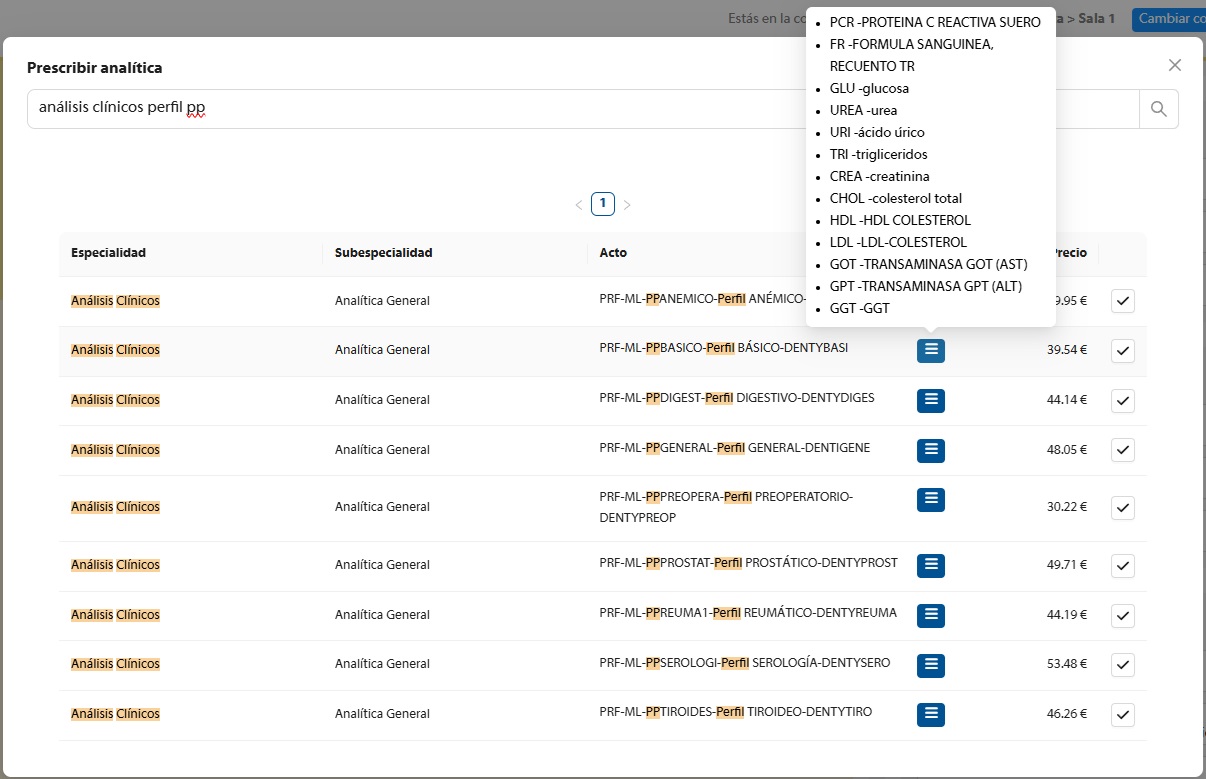
As part of the general prescription module, we have the following functionalities associated with the prescription of analytics:
3.1 Test prescription module:
- Prescription of simple and complex determinations. Complex determinations are sets of related simple parameters (clinical sets).
- Prescription by profiles.
- Intelligent prescription assistant. Prescription rules (incompatibilities, complementary, additional information).
- Intelligent Assistant personalized to the patient’s medical conditions (pathologies associated with the patient, ICD, others…).
- This module can be integrated into the HIS used by the prescriber.
3.2 Test Repository Module.
- Prescription registration Web services.
- Web service Authorization flyer (for authorizing centre).
- Web services analytical consultation.
- Web services collection of analytical results (PDF and detailed file).
- Web services analytical results query.
- Nomenclature conversion service.
Regarding the registration of the prescription, the basic data from the Prescription Registration Services Module (PRSM) are sent to the General Repository for registration using Web Services. These data are:
- Patient ID (card, NIF, NSS, etc).
- Insurer/Funding Entity.
- Prescribing doctor ID (member number).
- Set of parameters/determinations (1:N).
- Provisional diagnosis.
- Additional information (weight, sex, age).
3.3 Non-pathological analysis services.
It is also possible to generate non-prescribed voluntary analytical services not related to a pathology, requested by the patient and at the patient’s expense, e.g. genetic tests. Analyses of special services not prescribed and charged to the patient.
3. Summary
Eliminating paper and data entry and retrieval in the analytics management process is a key improvement in the new digital analytics process, but the model we are presenting goes much further, enabling the ability to provide intelligent prescription assistance for, for example:
- Search for the best analytical options for the patient/diagnosis.
- Analysis of the results together with personalization and consideration of each patient’s own medical circumstances.
The value and quality of the digital tests service will not only result in cost reduction and overall efficiency, but will also provide a truly different and friendly user experience for the patient.