1. Suffering in the authorization of services
Undoubtedly, one of the most painful moments in a health insurer’s customer experience is the request for authorization of a service. This process continues to require the intervention of the patient, often at a vital moment of weakness as they face treatment for an illness that drains their resources and energy.

The patient has to deal with a bureaucratic procedure that is familiar to the insurance company, but unfamiliar, or at least confusing to the patient. This often involves discussions with the insurance company and the service provider in order to obtain the authorization that is being requested. Moreover, during these procedures, it is not uncommon for there to be a lack of empathy with the patient who is forced to act as an intermediary between the doctor – the medical services providing the treatment – and the insurance company – the managers on the phone, without precise guidance from either side.
Bearing in mind that most health insurance companies work with a network of contracted facilities, we can ask ourselves the following question: Is it so difficult for the doctor or the centre contracted by an insurance company to request authorization directly from the insurance company itself, exempting the patient from having to go through this procedure?
No, it is not difficult. As almost always, it is technologically feasible and what it requires is a business strategy aligned with this objective. So how would it be made possible?
2. The Global and General Prescription Repository
Insurers talk about their network of contracted resources, but in reality, what we usually refer to as the company’s medical staff is not a network. These company facilities lack the connection and intercommunication required for a true network that shares information and services. In more than a few cases, this network is a mere list – even if it is displayed on the company’s website – with more or less accurate and updated information on the providers who can attend to their policyholders.

One way to feasibly and pragmatically improve this networking, and thus the authorization process, is to create a mechanism for information exchange between providers and insurers. This mechanism would consist of a GLOBAL AND GENERAL PRESCRIPTION REPOSITORY.
Some basic clarifications on the Global and General Prescription Repository:
- We speak of a GLOBAL repository because it is a single repository to which all insurers, providers and service providers that adhere to this authorization model would be connected.
- We speak of a GENERAL repository because it must contain all types of prescriptions or medical orders that can be carried out by a provider: analyses, diagnostic tests of any speciality, treatments, interventions and even referrals to other specialists.
- The idea is that a doctor from the patient history or specific software, sends the prescription directly to the General Repository and subsequently, the corresponding company can access and manage it.
- This repository shall be available for the potential performer of the prescribed service to receive authorization and even to report on the outcome of the service or test.
- The most disruptive aspect of the model is that the user or patient is freed from the authorization process.
This scheme is conceptually analogous and similar to the current Homologated Electronic Private Prescription – EReceta Delonia. To exemplify this parallelism:
- In the pharmacy prescription, prescribing agents generate prescriptions in the repository and pharmacies access and dispense the treatments to the patient.
- In the general prescription model, prescriptions are generated in the repository by medical professionals and accessed by the patient’s insurance company to authorize, reject or condition the service and inform the prescribing professionals and the insured.
3. Prescription Management System Modules
The Prescription Manager system consists of two basic functionalities:
- The prescription registration services module (registration discharge).
- The repository services module (cloud storage).
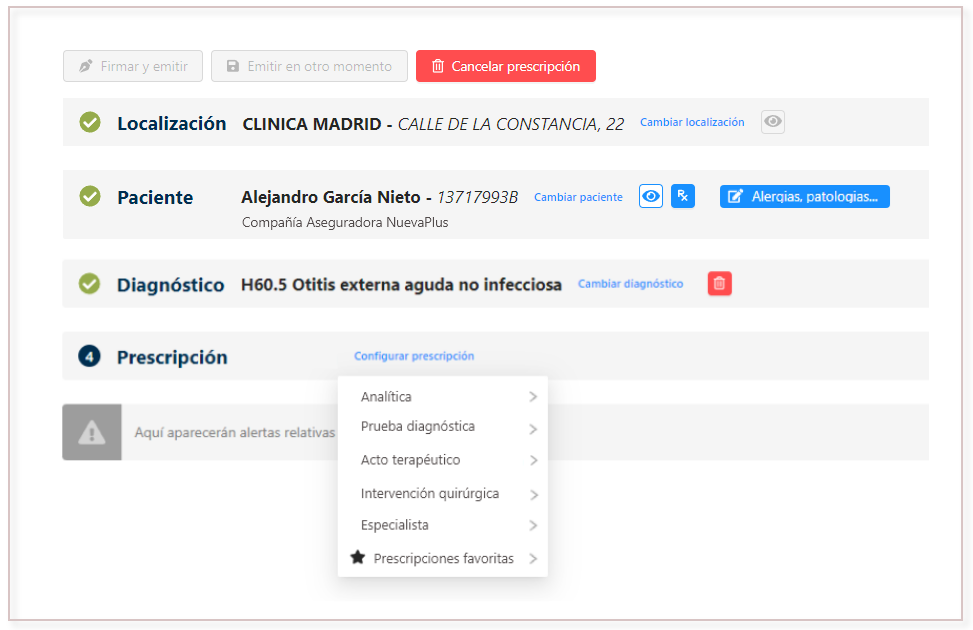
A. Prescription Registration Services Module (PRSM).
Normally, the Clinical HIS used by the prescribing service provider records the patient’s prescriptions or medical orders internally. It implicitly uses its own gazetteer – coded or not – or a description of the test or procedure.
This prescription is sent to the General Repository for registration using MSRP Web Services. The basic data it will have are:
- Patient ID (card, NIF, NSS, etc.)
- Insurer/Financier
- Prescribing doctor’s ID (member number)
- Nomenclator code
- Description of test/procedure
- Provisional diagnosis
- Additional information
B. Module Management Services Repository (MSGR).
Once stored in the repository, the prescription will be available for the insurer to access and manage according to its operational procedures. Three considerations:
- The insurer may manage the authorization of the prescription automatically or manually.
- The insurer may propose to the insured person an appointment or a professional to carry it out.
- The insurer may inform the insured of the procedures involved by any means it deems appropriate, in fact, it is appropriate to keep the insured informed of the process beyond the final resolution of the authorization.
This MSGR module will provide services such as:
- Prescription data information services
- Conversion of nomenclature Prescriber-Insurer
- Prescription status update service
- Services for permitted operators
- Service for the collection of results from the operator
4. Prescription Management System Flowchart
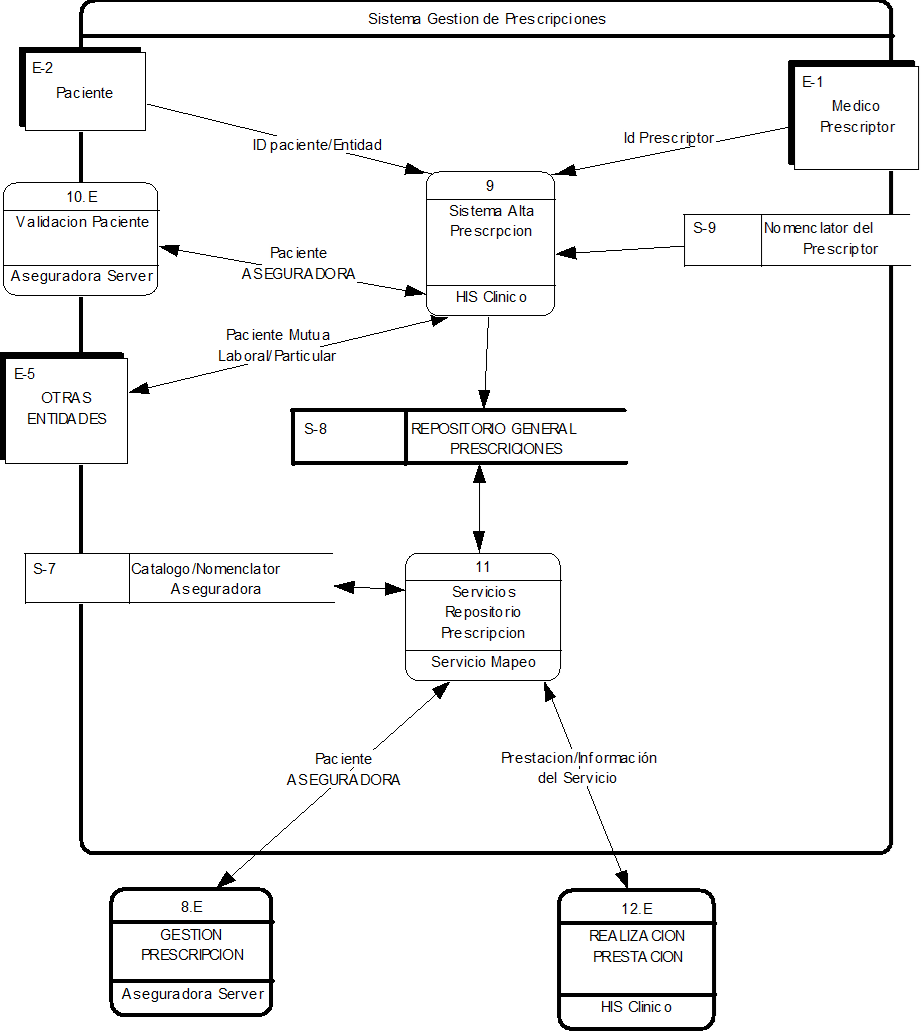
The flowchart of the Prescription Management System provides an overview of the model. Three points to clarify:
- As depicted in the flowchart, in addition, patient validation services (external process ‘10.E Patient Validation’) can be provided, provided that the Insurer has published web services of this type.
- The external process ‘8.E Prescription Management’ corresponds to the interconnection with the Company’s Authorization Centre. Ideally, it should be a synchronous/asynchronous authorization system so that direct automatic (on-line) authorizations can be processed and others (generally the more complex ones) asynchronously, to be managed by the Entity’s back-office.
- The provision of services’ process would correspond to the connection with the provider or professional who carries out the prescribed service, where, in addition to collecting the information on the prescription, he/she would return the result of the prescription so that the repository could serve it to the insurer/patient.
In short, sparing the insured patient the administrative burden of authorising services will significantly improve their patient experience, as well as their overall perception of their company. Likewise, insurers and their medical providers also significantly increase their efficiency by improving the procedure and reliability of the authorization process. It should not be forgotten that this process has a direct impact on the subsequent management of the billing associated with these authorized services.